A colleague asked me if I had any information on the use of Medication Therapy Management (MTM) as a way to reduce healthcare cost and prevent, or decrease, readmissions.
I’m kind of a digital packrat and I knew that I had some stuff sitting in Evernote, so I spent the better part of a day rummaging through the information I had. The deeper I dug the more I realized that MTM is a no-brainer. There’s enough information out there to convince even the staunchest opposition.
Some thoughts I had as I read through my Evernote notes:
- I find it interesting that we’ve coined the phrase Medication Therapy Management (MTM) for something that pharmacists have been doing for decades. I remember interning for a community pharmacy back in the late 90’s. Speaking to the patient about their medication, adherence, compliance, adverse effects, etc was simply part of the job. Have we forgotten about that?
- MTM comes in many forms. Positive intervention can be achieved over the phone, via Telepharmacy, face-to-face with a pharmacist or technician, and so on. It is not a one size fits all approach.
- Even the simplest interaction between provider and patient can create a positive impact.
- MTM should start when a patient is admitted for any condition, continue throughout their hospital stay, and follow the patient out the door to their homes. In other words it should be continuous.
- Not everyone will need pharmacist intervention once they leave the hospital. Healthcare systems should first target patients with chronic conditions, problems with cognition, poor history of compliance, or a heavy medication burdens. Like everything else in the world around us, some people will do better with more help while others will prefer less.
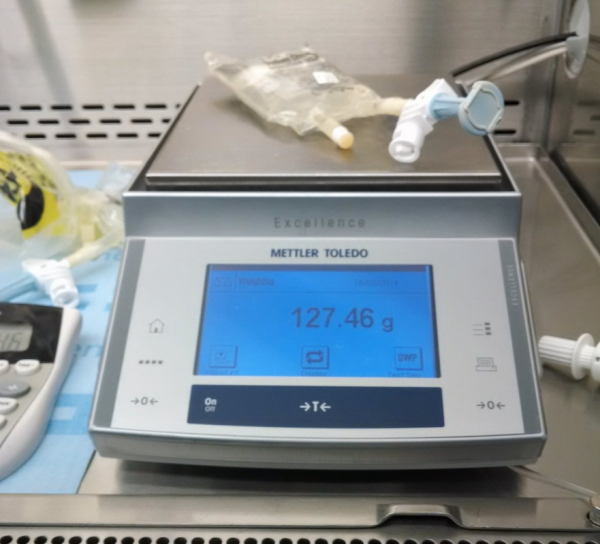
- mHealth and sensors should be part of MTM. Continuous glucose monitoring, heart monitors, blood pressure sensors, smart bottles, devices to monitor and record inhaler use – classic area for pharmacist intervention, wireless digital scales for weight – think heart failure, and so on . This information should be fed directly into the patients MTM record for review by the pharmacist, physician and nurse.
Below is a summary of the MTM information I sent my colleague.
(more…)
 Several months ago I wrote about
Several months ago I wrote about  I received an email this morning from Medscape introducing me to their new
I received an email this morning from Medscape introducing me to their new  There’s an interesting article in the
There’s an interesting article in the