I love pharmacy IV room workflow and technology, but I don’t get to talk about it much anymore. Most of my conversations these days are focused on IV room regulation, i.e. compliance with USP <797>/<800> and Board of Pharmacy rules.
So you can imagine my surprise when two people approached me on two completely different occasions at two unrelated events asking my thoughts on IV room technology. Awesome! Then they asked me what I thought about using robots in the IV room. Bummer. Of all IV room technologies, robotics is my least favorite.
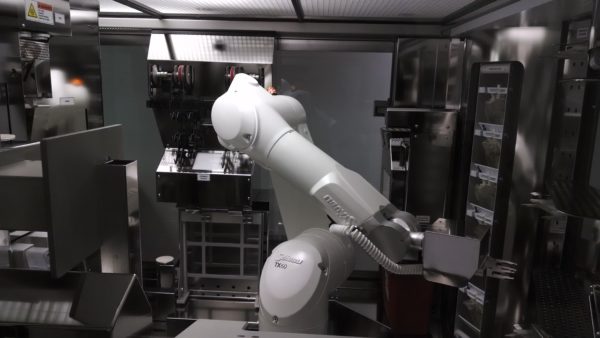
Ten years ago, I was optimistic about IV room robots. Today, not so much. If I could sum up my opinion in one sentence, it would be that highly-automated robotic systems for sterile compounding are not ready for prime time.
Note that I said highly-automated and not fully-automated. Even though robots replace human hands for the actual compounding process, they are dependent on human hands for moving products in and out of the robot before, during, and after the compounding process.
When considering IV robotics, one should always think about:
Patient safety – Can robots reduce CSP errors? Certainly, but so can most any IV room technology that utilizes bar-code scanning, gravimetrics, imaging, etc. Often times people will tout robotic systems for consistently compounding drugs within 5% of the prescribed dose. It’s not really a big deal. Doses slightly outside the 5% range are not clinically significant, and getting it within that range is not important enough by itself to warrant the investment in a robotic system. Given proper guidance and a system for compounding, particularly an IV workflow management system, humans can easily be as accurate.
Worker protection from hazardous drugs (HDs) – There is no question that IV robots have the potential to reduce worker exposure to HDs during the compounding process. Then again, new USP <800> guidelines do the same. Ever heard of a CSTD?
Workflow efficiency – Not sure a robot brings you increased efficiency unless you’re talking about single batch high-volume IV production. I sat for hours watching IV robots doing their thing in pharmacy cleanrooms across the country. I don’t think I ever thought to myself, “dude, that thing sure makes things easier/betterâ€.
Cost reduction from moving outsourced CSPs back in house, i.e. no longer having to purchase CSPs from a third party – Not specific to robots. Perhaps for single batch high-volume IV production, but doubtful.
Reduced waste from discontinued orders falling off work queues before they are filled – Sure, a robot can help with this, but the same is true for almost any IV workflow management system.
Comprehensive documentation for regulatory compliance – These systems certainly collect lots of data but how easy is it to use? Just because the system collects info doesn’t mean you can get it out when you need it. I’ve seen things. Just sayin’.
Return on investment (ROI) – What do these systems give back? There are few pharmacies where IV room robots will result in a positive ROI. I’ve seen pharmacies try. While their arguments may sound good on paper, in practice they are as thin as the paper they are written on. The only time these systems yield a real ROI, in my opinion, is when they are used to repetitively compound the same few items over and over again – in other words, batch compounding for high-volume items. All of the systems have roughly the same throughput, which is much lower than that of a highly skilled technician. IntelliFill i.v. is the fastest of all the robots I’ve seen, but it is limited in scope to syringes.
Formulary limitations – One of the major limitations of IV robots is the number of formulary items they can handle. During visits to facilities using IV robots — San Francisco, CA; Asheville, NC; Baltimore, MD; Madera, CA; and so on — I saw very few medication “line items†assigned to the robot. The largest number I witnessed was somewhere around 10, and the smallest number was two. Two! Someone had a million-dollar robot making CSPs out of two drugs. Hospital formularies are large and diverse. They include all kinds of IV products: piggybacks, large-volume parenterals, syringes, and so on. Not to mention that formularies change all the time. The inability of these systems to manage a large number of different CSPs at one time is definitely a limitation.
Maintenance – What does it cost to maintain these bad boys? They don’t operate on a zero cost. They also don’t maintain themselves. Operational resources required for things like robot maintenance, formulary maintenance, product changes, and so on are important considerations to keep in mind when purchasing a robot. Who is serving who…. or is that who is serving whom? I can never get that right. Anyway, the time, energy, and effort required to keep an IV robot at peak operational efficiency simple isn’t worth it. At least not in my opinion.
In a nutshell, I’m just not a fan of the current crop of IV robots. Does that mean that there is no future for robots in sterile compounding? On the contrary, I think we must move toward a future where all CSPs are made by robots. It’s the only thing that makes sense. Unfortunately, that future is still far off.
I’ve had the opportunity to peak behind the curtains at a few robots currently under development. There are some great products coming down the pike, but we are going to have to wait a while. Apparently, building robots with creative new features is hard.





