I’ve been writing about the need for pharmacy integration for years. Most of it negative, and deservedly so because it’s been lousy.
With that said, things appear to have changed in recent years. Integration, it seems, has slowly become a thing. Maybe because I’ve been out of general pharmacy practice for so long that it seems decent, or maybe it’s getting better. Hard to tell, honestly.
Pharmacy systems aren’t really talking to each other better than before, per se, but the number of disparate systems seem to have decreased over the years. Once there were many, now there are seeming few. Once, everything was “best-of-breed”, now things are moving to one system to rule them. Case in point, electronic health records. (EHRs).
I always thought pharmacy integration would take place from the inside out, i.e. pharmacy systems would integrate with other systems and drive information sharing across the hospital. Not even close. Instead, pharmacy systems have become more integrated by being consolidated and sucked into the EHR.
The advent of EHRs has done more for system integration in healthcare than just about anything else. I have plenty of negative things to say about EHRs, but it’s clear that they’ve changed the way we practice, forever.
The way I see things, at least now, most healthcare systems have fallen into two large buckets: 1) documentation, clinical, and other; and 2) operational logistics.
Clinical Documentation: Clinical documentation used to take place in “the chart”, among many other places. The chart was nothing more than a binder filled with dividers, separating one bit of information from another. Think of a Trapper Keeper, minus the cool picture on the cover. Paper was everywhere. If you wanted to read something about a patient, like a progress note or radiology report, you had to go to the chart, which wasn’t always easy. They had a way of walking away with physicians and not making their way back to the nursing station.
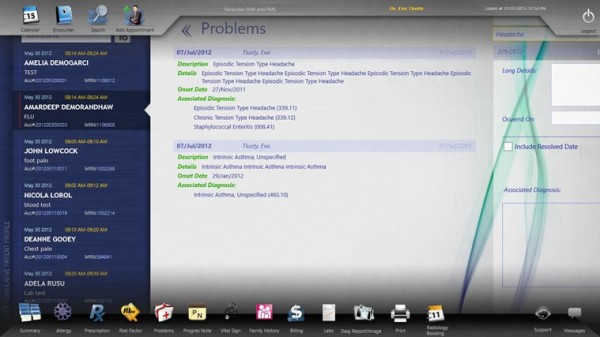
This all changed when EHRs hit the scene. Everything from demographic data to notes, lab values, medication information, and so on is at your fingertips. If you need information, all you do is log into the EHR and go hunting. Admittedly, it’s not as easy to navigate as a paper chart, but it’s a heck of a lot more data rich and never walks away.
Most of the information coming out of hospital pharmacies these days can be found in EHRs. That includes medication distribution information, pharmacist notes, barcode archives, and so on.
Operational Logistics: Think Amazon warehouse. That is the easiest way I can explain pharmacy logistics. You buy something from a third party, store it in the pharmacy for a period of time, and send it to a patient when it is ordered. Simple, really. We are still not very good at it, but that’s the gist.
For the most part, pharmacy logistics has maintained its distance from the influence of EHRs. Instead, inventory management has been driven largely by a other, non-EHR companies: CareFusion, Omnicell, and to a lesser extent, Swisslog. These companies have grown and expanded over the years, increasing their portfolios to cover more and more areas of the pharmacy.
I have mentioned the “four areas of pharmacy” many times: standard storage, refrigerated storage, controlled substance storage, and the iv room. The first three areas are still dominated by these companies. Carousels, inventory software, refrigerators, various cabinets controlled by remote locks, and automated packagers can be found in most large pharmacies. All of which are offered by the aforementioned companies. There was a time when it was common for any number of these products to be supplied by different vendors. Not so much anymore.
These days, it is all about integrated systems from a single vendor. When given a choice, pharmacies are deciding to purchase from a vendor that can “do it all”. For example, CareFusion offers Pyxis ES ADUs for medication distribution at the point of care; Pyxis Logistics software and hardware for medication distribution from the pharmacy; Pyxis CII safe to manage controlled substances; BD Cato for the IV room; and so on.
With that said, the IV room is in a state of flux. The nature of this area lends itself to both operational logistics and documentation, the latter of which seems to be more important now more than before. It may be the only area of the four where inventory management means less than documentation. I expect this trend to continue. Â
Surprisingly, I really have seen better integration amongst pharmacy systems these days. I fully expect it to improve even more as EHRs expand and eventually creep into operational logistics. At least one EHR vendor has already made a significant impact in the IV room. Eventually, pharmacy will be just another department within the EHR’s web of control. I see both good and bad in such a future, but that’s a blog post for another time.