Both ISMP and ASHP are working on draft recommendations for technology in the IV room. ISMP’s version is an update to their ‘Guidelines for Safe Preparation of Sterile Compounds’ that was originally published in 2013. The proposed revision is open for public comment until April 10th. ASHP is also working on new recommendations for the use of IV Workflow automation technology for the preparation of compounded sterile products (CSPs)
It feels a bit like running into a burning building to pull people out instead of taking action to prevent the building from catching fire in the first place, i.e. reactive instead of proactive. Many of us have known for years that there’s a problem in the IV room. It’s the dirty little secret of the industry. We’ve been saying that change is needed, but it has mostly fallen on deaf ears until now. What’s changed? I have an opinion, but that’s for another time.
We’ve known for decades that the IV room is not only one of the busiest areas in a pharmacy but also one of the most dangerous. IVs present higher risks than most other medications and the literature presents abundant evidence of the prevalence of pharmacy compounding errors, (1, 2, 3, 4, 5, 6, 7) which result in patient harm or death. (8,9, 10, 11) These errors not only impact patients but caregivers and healthcare facility as well. The human and financial toll are staggering.
While we may think we don’t make mistakes in the IV room, studies have shown that errors during CSP production are not uncommon. According to the frequently cited article by Flynn, Pearson, and Baker published in 1997: “A five-hospital observational study on the accuracy of preparing small and large volume injectables, chemotherapy solutions, and parenteral nutrition showed a mean error rate of 9%, meaning almost 1 in 10 products was prepared incorrectly prior to dispensing.†(7)
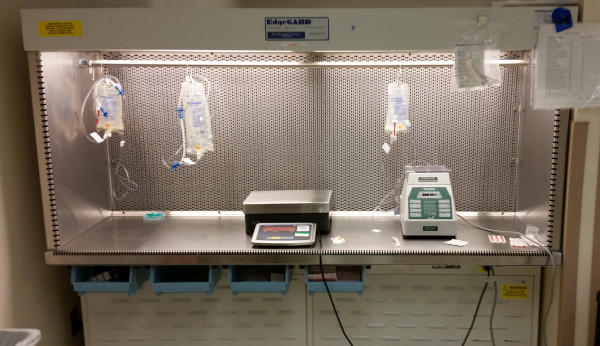
Many of the errors found with CSPs can be easily prevented through the use of common, currently available technologies. While adoption of technology has been slow, pharmacies are increasingly moving toward the use of these systems. Guidelines from ISMP and ASHP will certainly help speed things up.
Compliance with USP <797> Pharmaceutical Compounding—Sterile Preparations and ASHP Guidelines on Quality Assurance for Pharmacy-Prepared Sterile Products has certainly led to improved processes and safety in the IV room. Both address the need to accurate identify, measure, dilute, mix, package, and label CSPs. However neither of the guidelines is designed to drive adoption of CSP technologies to improve safety, accountability, and documentation.
The quality and safety of CSPs goes beyond sterility, potency, and stability and must include accurately identified and measured ingredients, diluents, final solutions, and containers as well as identifying, tracking, and documenting the CSP from cleanroom to patient. Current practices do not support or encourage the use of available automation and technologies to support these activities.
Much has yet to be defined and there are currently no guidelines or governing entities to drive standardization for vendor development and design, nor is there anything to help healthcare systems make smart choices.* With that said, it appears that changes are just around the corner.
During this time, it is important to understand the following:
- Vendors must design – and users chose – systems that provide a clear advantage over manual systems in patient safety, workflow standardization, and documentation; are cost-effective; interoperable with existing systems; are simple to install, use, and maintain; and carry a high degree of certainty and reliability.
- Minimum requirements** should include interoperability with pharmacy information systems and electronic health records, control of final product label, bar code verification of all ingredients and final containers, imaging for verification and documentation, documentation of master formula records, lot numbers, expiration dating, and products used, and basic dose tracking functionality.
- While some of the products available today generate their own ISO class 5 compounding environment, these systems must function properly in cleanroom environments and comply with all USP <797> and <800> standards and recommendations.
- And finally, technologies for CSP production must be correctly selected and utilized to effectively create a safe environment for both the healthcare provider and the patients they serve. There is no one-size-fits-all approach to these systems and each healthcare system is different. Proper selection will depend on several factors.
It’s time for vendors and healthcare systems to wake up and get ready for what’s coming.
References
- US Food and Drug Administration Website. Report: Limited FDA Survey of Compounded Drugs. Available online at: http://www.fda.gov/cder/pharmcomp/survey.htm. Accessed on January 3, 2004.
- United States Department of Justice, Federal Bureau of Investigation Website, April 22, 2002. Available online at: http://kansascity.fbi.gov/kcmostate042202.htm. Accessed on July 6, 2002.
- Trissel LA. “Compounding our problems–again.†Am J Health-Syst Pharm. 1 Mar. 2003: 432.
- Selenic D, Dodson DR, Jensen B et al. “Enterobacter cloacae bloodstream infections in pediatric patients traced to a hospital pharmacy.†Am J Health-Syst Pharm. 2003; 60:1440–6.
- Niedowski E, Bor J. State to probe Hopkins death: 2-year-old cancer patient died after receiving improper IV mixture. December 20, 2003. Baltimore Sun, Baltimore, MD.
- Flynn, EA, Pearson, RE, Barker, KN. “Observational study of accuracy in compounding IV admixtures at five hospitals.†Am J Health-Syst Pharm. 1997 Apr 15; 54: 904–912
- Solomon SL, Khabbaz RF, Parker RH, et al. “An outbreak of Candida parapsilosis bloodstream infections in patients receiving parenteral nutrition.†J Infect Dis 1984; 149:98–102.
- Hughes CF, Grant AF, Leckie BD, et al. “Cardioplegia solution: A contamination crisis.†J Thorac Cardiovasc Surg 1986; 91:296–302.
- Associated Press. Pittsburgh woman loses eye to tainted drug; 12 hurt. Baltimore Sun. November 9, 1990:3A.
- Dugleaux G, Coutour XL, Hecquard C, et al. “Septicemia caused by contaminated parenteral nutrition pouches: The refrigerator as an unusual cause.†J Parenter Enteral Nutr 1991; 15:474–475.
- Perrin J. “Unsafe activities of compounding pharmacists.†Am J Health-Syst Pharm 1995;52:2827–2828.
*Actually, I would argue that IN THE CLEAN ROOM: A review of technology-assisted sterile compounding systems in the US (Jerry Fahrni, Pharm.D. and Mark Neuenschwander) would be a great tool for helping pharmacies make smart choices, but most seem averse to the information.
**Minimum requirements. This is not to say that this should be the end game, but rather a place to start. Overreaching in the beginning of this process is sure to dampen development and adoption.