Several years ago there was a debate over the long-time practice of having pharmacists review all medication orders prior to administration; referred to as nearly universal prospective order review (NUPOR).(1) At the heart of the debate was whether or not such a process was still relevant in the changing face of healthcare, i.e. do pharmacist really need to see every single medication order prior to that medication being administered to a patient?(2)
The argument in favor of universal medication order review is obvious: ensure complete, accurate orders. The argument against universal medication order review is that it’s expensive, time-consuming, and unnecessary in most instances. My own personal belief is that the practice is antiquated and should be changed.
The introduction of electronic health records (EHRs) has changed the medication order entry landscape. No longer do pharmacists interpret and enter orders from hand-written orders on paper faxed to the pharmacy. Those days are mostly behind us. These days, medication orders are generated electronically from pre-defined, pre-built entries in the EHR. Providers simply check a box and bam, order entered. Or as one pharmacist put it in a discussion forum recently “I mean an order set that has been checked by pharmacy, checked by a physician, checked by nursing, approved by P&T / Medical Ethics ….how many times do we need to verify it?â€. I feel the same way.
In the rare case that no checkbox is available, today’s EHRs are intelligent enough to provide directions for the user. Not to mention that a majority of medication orders processed in a hospital are simple, routine, and require no critical thought. It is the exception rather than the rule to see an order that requires any deep thought or intervention.
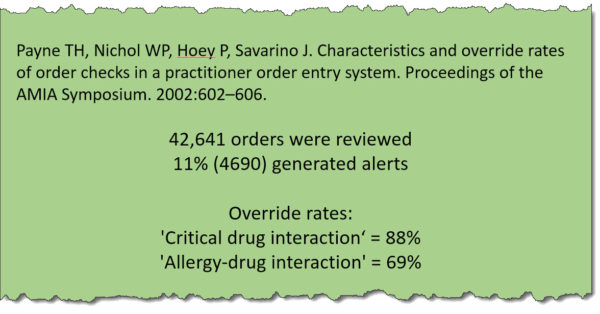
There are those that argue that taking pharmacists out of the order verification role is dangerous, but nothing could be further from the truth. Having pharmacists verify orders is retroactive, at best. What percentage of orders require a pharmacist’s intervention? 10%? 5%? Hard to say, but the percentage is small.(3) The same pharmacist mentioned above said it best: “I did a cursory look and for one month out of 150,000 orders verified, only 5,000 had an intervention performed on them. So 3% of the time we are actually doing something significant enough to warrant an intervention.†So current best practice has pharmacists — a highly trained, expensive professional — looking at 100% of orders in an attempt to find the 3% that have problems. Seems kind of silly.
I often look to the model used in poison control centers for support of my opinion. Non-pharmacists screen calls at poison control centers. If the call can be handled via a well-thought-out algorithm, then it’s handled. If not, the call is escalated to a pharmacist. In other words, pharmacists are only getting the calls that require their particular brand of expertise. That’s poison control! Think about it.
The days of having a pharmacist look at each and every medication order entered into an EHR are over. It’s an antiquated process that’s long overdue for an overhaul. The time has come for healthcare systems to make better use of their personnel.
—–
- People love their acronyms. I’ve always called it “order verificationâ€.
- The answer is obviously no, pharmacists do not need to review every single medication order before that medication is given to a patient. But, people like to argue.
- I’ve said many times that a monkey could do my job. While my comments are flippant, the sentiment rings true. I could train an intelligent teenager to do 80% of my job in a couple of short weeks. On a side note, I’ve never had a single person challenge me regarding my monkey comment. Seems odd, don’t you think? I mean, it’s insulting.