This morning I woke to the news that No Syringe Is Approved as a Standalone Storage Container, FDA Says. This I’m sure is in response to the recent issue with BD syringes and drug stability. I need to think about this more, but my gut reaction is that this is huge and will have a significant impact on many acute care pharmacy practices across the country.
There are three factors to consider when making and dispensing compounded sterile products (CSPs): accuracy, sterility, and stability.
Accuracy. Self-explanatory. When you make a CSP you want it to be as accurate as possible. This is where I believe automation and technology come into the equation. My thoughts on the subject can be found in many essays/articles published on this site.
Sterility is covered ad nauseam by USP General Chapter <797>. CSPs should be free of microbial contamination. This, of course, is for the safety of patients receiving treatment with CSPs. If you have any questions regarding how long something can be stored following compounding, and still be considered “sterile†then you should look no further than the beyond-use dating (BUD) guidelines found in <797>.
Stability. When you store something in a container, i.e. a syringe, bag, bottle, etc. you want the drug to remain active for as long as necessary to administer to the patient. We know that some drugs are sensitive to light, temperature, type of storage device, etc. However, pharmacy has long used syringes as a method of distribution, and as long as the drug was considered unaffected by light and temperature, not much consideration was given to stability.(1) This is a holdover from the days when we, i.e. pharmacy used to draw everything up in glass syringes. Glass was an awesome storage medium, but we didn’t really change out practice when glass syringes became too expensive to be practical and we went to plastic. While addressed in USP General Chapter <797>, stability is not given the same detailed coverage as sterility. USP <797> was never meant to address stability in great detail.
Recently I’ve seen an upward trend in pre-drawn syringes. I’ve spent the better part of the last three months immerging myself in what goes on with medication distribution and use in the O.R. That is to say I’ve been educating myself on processes and paradigms of how anesthesiologists and pharmacy work together to ensure safe, accurate and responsible medication use during surgery.
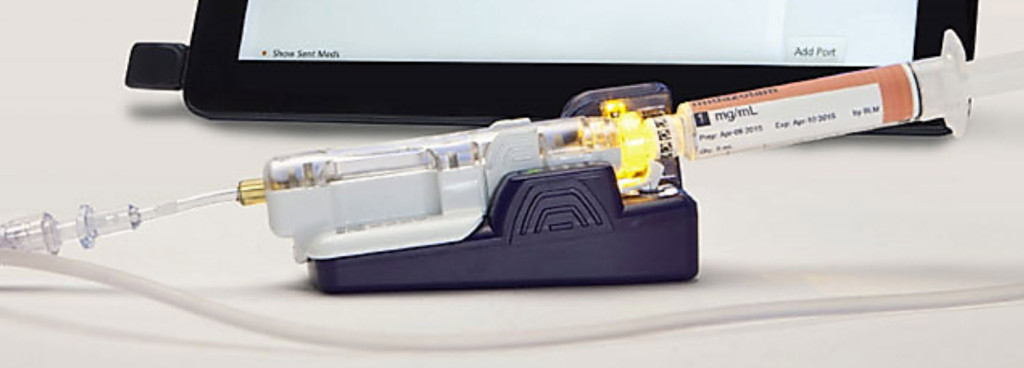
One of the major trends I found in O.R.’s was the use of pre-drawn syringes. Pharmacy likes them because it gives them more control over drug usage and waste, and anesthesiologists like them because they don’t have to draw medications from vials prior to administration. Anesthesiologists are more concerned with monitoring the patient then they are with having to deal with medication labeling, etc.; and rightly so.
This desire to supply anesthesiologists with pre-drawn syringes has created an interesting side effect in CSP automation – there is a renewed interested in CSP robots in the clean room. Robots are good at batch production. Pulling several hundred syringes filled with the same drug is an ideal use for a compounding robot.
This of course, doesn’t include pediatric facilities that use pre-drawn syringes to stock their shelves to meet the needs of their patient population. I remember when I was a pediatric pharmacist back in the early 2000’s. We pulled thousands of syringes each and every day to replenish stock not only on our shelves in the pharmacy, but to place in ADCs for easy access to medication for nurses and physicians.
Some pharmacies will use third party vendors like PharMEDium for their pre-drawn syringes. I bet companies like PharMEDium already have data on the stability of drugs stored in syringes. Will they share this information with the rest of the pharmacy world? My gut reaction is that they won’t. By sharing  information they’re basically cannibalizing their own sales. What’s this do for them? Uptake of customers and bigger sales in the immediate future. It’ll be interesting to see how they handle it. Not to mention potential liability snafus.
Like I mentioned above, I need to think on this more deeply. However, at this moment I’m thinking that the FDA’s stance on syringes as stand-alone storage devices is going to create a lot of headaches for pharmacies across the country over the next several weeks. It’ll be interesting to see how organizations like ISMP, ASHP, USP, etc. respond to the FDA’s statement.
Grab some popcorn folks, this should be good.
——-
- There’s much more to this statement, but for the sake of brevity let’s just leave it at that.