The differences between stability, beyond-use date (BUD), and expiration for compounded sterile preparations (CSPs) causes a lot of confusion. I’m not even certain that I fully understand their roles in day to day pharmacy operations. With that said, I think the key is for everyone to at least understand and agree that the BUD of a CSP is not the same as the expiration date.
Here’s how I understand it:
Stability is based on the chemical stability of the solute in solution, i.e. ingredients alone or in combination. This is what the Handbook on Injectable Drugs is all about, i.e. loss of drug potency/activity in solution.
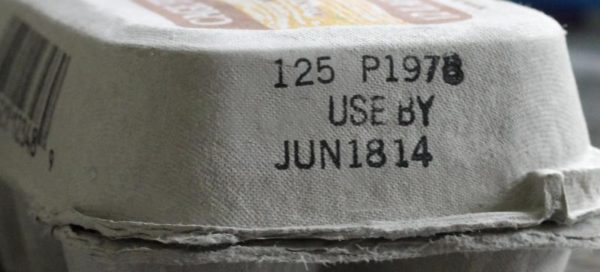
Expiration date is defined by the FDA and identified by the product manufacturer.  Basically, it’s the shelf-life of the drug when properly stored. The expiration date no longer applies once the manufacture’s container is opened and the drug product is transferred to another container for dispensing or repackaging. Pharmacy uses “expiration date†loosely as we are not manufacturers. Most often I see pharmacies use expiration date in place of stability, i.e. the drug is good in solution for “this longâ€.
Beyond-use date (BUD) is assigned by the pharmacy for a CSP and is an arbitrary date/time found in USP <797> and adopted by many boards of pharmacy. BUD is based on sterility, stability. The BUD identifies the time by which a preparation – once mixed – must be used, i.e. “hungâ€. Once the CSP is hung on a patient, the BUD goes out the window and no longer applies. USP <797> does not address what to do with a CSP once it is hung on a patient. So something can have a BUD of 12-Hours, but be stable much longer. Pharmacies can extend BUDs, but only after independent sterility testing performed according to USP <71>, or in some cases when appropriate literature sources are used.
In summary, the BUD is not the expiration date, nor the stability of a preparation. Nurses must hang a CSP before the BUD is reached. The CSP can continue to hang on the patient until the “Expiration Date†is reached.
I would love to hear how facilities are dealing with these three concepts. Does your facility use a BUD and expiration on CSP labels?