I was rummaging through my travel bag and found some items that I collected during the ASHP Summer Meeting back in June. Most of the information had to do with IV room systems, tablet identification, and so on. But there was one item that caught my eye that didn’t fit with the rest: color labels.
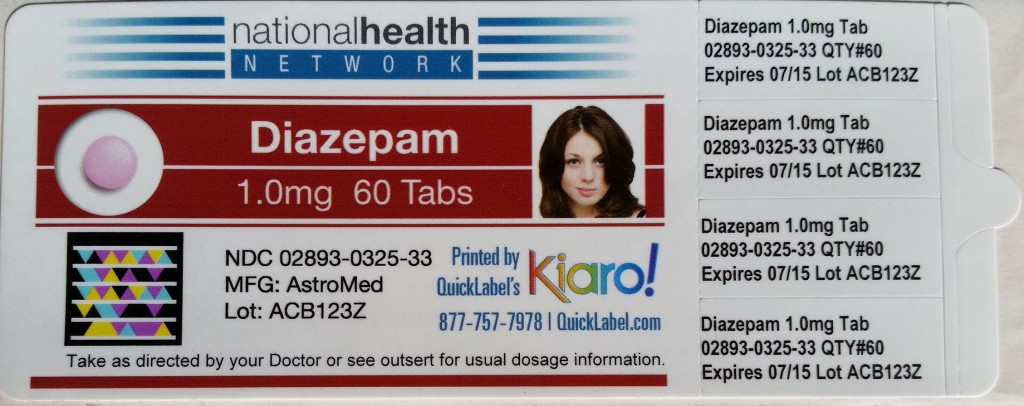
I’ve written about the use of color on pharmacy labels before. It has its place, but in my opinion the major barriers have been cost and label quality. That’s why I was so interested when I saw the booth from Quick Label Systems at the ASHP Summer Meeting. The labels they had on display were spectacular. It’s difficult to see in my photo, but the image quality and label stock are top notch. The labels are tough –  really tough – resistant to water, and don’t smear. Very nice.
The quality of the label and print gives users the ability to place a crazy array of information on the label, including the ability to embed audio or links to video using bar code technology. It’s pretty cool.
The company isn’t a pharmacy solution in the traditional sense, but do provide OEM services for other companies. In other words, if you have a need for color labels Quick Label Systems will build color label printers with your name on them.
Not every product that leaves the pharmacy needs a color label, but they could certainly be useful in the IV room. Using color to differentiate or highlight something that requires special attention like chemotherapy is always helpful to pharmacy and nursing.
I’ll try to get the rest of my bag’s contents up over the next few days.
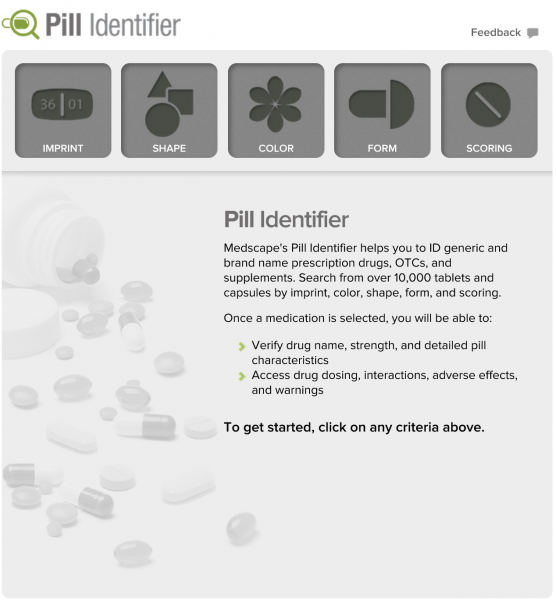 I received an email this morning from Medscape introducing me to their new
I received an email this morning from Medscape introducing me to their new  UCSF
UCSF