Last week I wrote about the tragic death of a patient caused by a drug error (CSP error results in death of a patient). One day later on December 18, 2014, ISMPÂ also addressed the error in the Acute Care edition of their biweekly ISMP Medication Safety Alert, i.e. one of their newsletter. I had hoped that ISMP was going to provide much greater detail and insight into the error, but that’s not the case. At least not at this point, anyway.
I had hoped to find out what occurred in the pharmacy to allow such a mistake to happen. Perhaps more details will come to light as time goes on. All we can do is wait.
With that said here are some things from ISMP worth noting:
“To prevent inadvertent use, identify neuromuscular blockers available within your organization and where and how they are stored. Regularly review these storage areas, both inside and outside of the pharmacy, including agents that require refrigeration, to consider the potential for mix-ups.”
“Limiting access to these products is a strong deterrent to inadvertent use. Consider limiting the number of neuromuscular blockers on formulary, and segregate or even eliminate storage from active pharmacy stock when possible.”
“Restrict storage of paralyzing agents outside the pharmacy and operating room by sequestering them in refrigerated and nonrefrigerated locations.”
ISMP recommends highly visible storage container for neuromuscular blockers (one example here: www.ismp.org/sc?id=458).**
ISMP recommends affixing warning labels on vials and admixtures that clearly communicate the dangers of neuromuscular blockers.**
ISMP recommends the use of IV workflow technologies. “Now is the time for hospital leadership to support the acquisition of IV workflow technologies that utilize barcode scanning of products during pharmacy IV admixture preparation.” While the article lists only three systems, there are several on the market [see  In the Clean Room TOC for a current list of many of the available systems].
————————————-
**I know that many think this is a good idea, but I’m not so sure that I’m one of them. On the surface, using highly visible storage containers and labels might seems like a good idea, but over time people become used to the idea and become blind to the differences. In addition, over the years the number of items that require alternate storage and labeling has grown, making differentiation “the norm”. It’s like the student that highlights everything in the textbook with five different colors. Eventually the entire book is highlighted, making the process meaningless to the reader.
 There’s an interesting article in the
There’s an interesting article in the 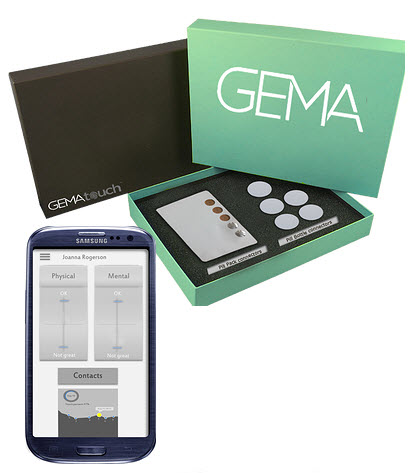 This is interesting, the use of NFC tags to track patient’s medication compliance. Makes sense when you consider the ubiquitous nature of NFC on mobile devices these days.
This is interesting, the use of NFC tags to track patient’s medication compliance. Makes sense when you consider the ubiquitous nature of NFC on mobile devices these days.