The June 17, 2010 issue of ISMP Medication Safety Alert I received has an interesting article on the unintended negative consequences of the Centers for Medicare & Medicaid Services (CMS) regulation requiring medications to be administered within 30 minutes of their scheduled dosing time. I’m sure that the CMS 30-minute rule was created with good intentions in mind, but in reality it creates a lot of anxiety and bad habits. According to the ISMP article, the CMS 30-minute rule “may be causing unintended consequences that adversely affect medication safety. While following the 30-minute rule may be important to hospitals, many nurses find it difficult to administer medications to all their assigned patients within the 30-minute timeframe. This sometimes causes nurses to drift into … unsafe work habits.†Those unsafe work habits include removing meds from automated dispensing cabinets (ADC) for multiple patients at once, removing meds ahead of time, falsifying documentation to meet the 30-minute rule and preparing doses ahead of time; all dangerous practices.
(more…)
Tag: Patient Safety
-
Is the 30-minute rule for medication administration good or bad?
-
IntelliDose EHR integration
CMIO: “Allscripts will integrate IntrinsiQ’s IntelliDose chemotherapy management tool into its EHR product suite as a new offering for physician practices.
The Waltham, Mass.-based IntrinsiQ’s IntelliDose calculates and tracks the administration of chemotherapy treatments and will enable Allscripts’ multi-specialty and oncology clients to manage oncology patient care workflow, according to the company.
Under the agreement, oncology practices will work with Allscripts account managers to coordinate with implementation and training specialists from the IntelliDose team. Integration of IntelliDose into Allscripts tools will enable Allscripts clients to select the add-on program to navigate patient records across both systems, IntrinsiQ stated. “
This sounds like an interesting concept. I tried looking for detailed information on IntelliDose, but really couldn’t find much. Based on information at the IntrinsiQ website it appears that IntelliDose is a clinical decision support system designed specifically for chemotherapy. Based on the description, IntelliDose does many of the same things that a pharmacy information system does, i.e. checks for “body surface area limitations, patient allergies, and exceptional lab results†in addition to reviewing “dosage variables such as ideal weight, serum creatinine, and creatinine clearance.†Sounds like a pharmacist.
-
More thoughts on standardization
 I’ve mentioned this before several times on this blog, but feel like I have to say it yet again; we need to start standardizing certain things about health information technology. The lack of standardization reared its ugly head at me again last week when our Pyxis med stations kept dropping medications off of patient’s active profiles. It appeared to always be the same drug, IV ketorolac. It took me a while to figure out the problem, but it turns out that Pyxis and our pharmacy system don’t agree on certain basic elements of time. Go figure.
I’ve mentioned this before several times on this blog, but feel like I have to say it yet again; we need to start standardizing certain things about health information technology. The lack of standardization reared its ugly head at me again last week when our Pyxis med stations kept dropping medications off of patient’s active profiles. It appeared to always be the same drug, IV ketorolac. It took me a while to figure out the problem, but it turns out that Pyxis and our pharmacy system don’t agree on certain basic elements of time. Go figure.
(more…) -
What’s wrong with this picture, err, I mean with these words?
I was reading an article in the most recent issue of Patient Safety & Quality Healthcare and I ran accross the paragraph below. I had to chuckle to myself. Would this be the definition of irony?
Feel free to comment on what you think is wrong with this paragraph. Don’t look too hard because it should be immediately obvious to all healthcare providers. I’ll update the post tomorrow.
-
A look at one pharmacists unwanted potential
A recent post by John Poikonen got me thinking about medication errors. They’re part of every pharmacists day, but we rarely give them much thought.
I’ve been a pharmacist for more than 10 years now and I’ve make my fair share of mistakes. I would like to think that none of those errors caused harm, but that would be naïve to say the least. And forget about the errors that were never detected because one can only speculate about those.
(more…) -
Lack of interoperability, standardization and simplification is risky
 I’m not a big fan of the using the “best of†model for hospital information systems (HIS). You know, when you buy the best pharmacy system you can find, and the best lab system you can find, and the best ED system you can find, and so on. All this does is create a giant headache for everyone involved because the systems don’t always play nice with each other, which means data gets lost or hijacked between systems by the Interface Noid. Data gets pushed, moved, shuffled, altered, chopped and converted, and it doesn’t always come out the way you intended. Or worse yet, you have a case where the systems aren’t interfaced at all.
I’m not a big fan of the using the “best of†model for hospital information systems (HIS). You know, when you buy the best pharmacy system you can find, and the best lab system you can find, and the best ED system you can find, and so on. All this does is create a giant headache for everyone involved because the systems don’t always play nice with each other, which means data gets lost or hijacked between systems by the Interface Noid. Data gets pushed, moved, shuffled, altered, chopped and converted, and it doesn’t always come out the way you intended. Or worse yet, you have a case where the systems aren’t interfaced at all.I recently heard of a case where a hospitals ED system wasn’t interfaced with the rest of the facilities information systems and disastrous results ensued. A patient came in through the ED with a very specific allergy; noted in the ED system. The information wasn’t available in the nursing or pharmacy systems. The patient was admitted and transferred to the floor. The little detail about the allergy wasn’t passed on during report and the patient ended up receiving that very medication based on the attending physician’s order. To make a long story short, the patient had an anaphylactic reaction and won a three day, all expenses paid trip to the hospitals intensive care unit.
I wonder how often things like this happen due to short sided HIS implementation and deployment. Technology might not be the answer to all our problems in healthcare, but you have to admit it certainly could have helped in this particular example.

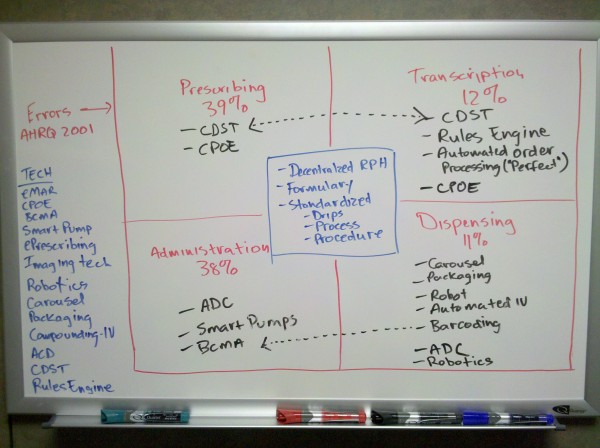
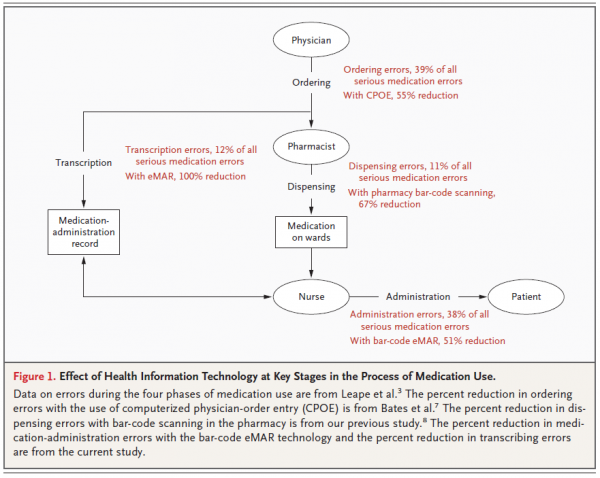
 Bar-code medication administration has been around for a while, but hasn’t gained the same notoriety as other forms of healthcare technology like computerized provider order entry (CPOE) and clinical decision support (CDS). However, it looks like the tide is starting to change as we’re currently in a unique position to see bar-coding from several different angles.
Bar-code medication administration has been around for a while, but hasn’t gained the same notoriety as other forms of healthcare technology like computerized provider order entry (CPOE) and clinical decision support (CDS). However, it looks like the tide is starting to change as we’re currently in a unique position to see bar-coding from several different angles.