Pharmacy informatics remains in its infancy as a profession. What started out as a job for tech-savvy pharmacists with working knowledge of pharmacy has turned into an ever expanding career field.
I’m looking through the ASHP Summer Meeting Informatics Institute schedule and the topics are varied. I see something on human factors, information management, clinical decision support, and e-prescribing. And that’s only on first glance.
If you look at job descriptions for healthcare systems seeking informatics pharmacists you’ll see everything from involvement in strategic development of services to data entry by monkeys, and everything in between. There’s little consistency in what one facility is looking for versus another. That point alone is telling.
This reminds me of pharmacy practice in acute care facilities 20 years ago. Outside of academic medical centers pharmacists were largely involved in operations, and only slightly involved in other care activities. That’s all changed as pharmacists practice in many different areas today and can specialize in a variety of disciplines, i.e. infectious disease, cardiology, etc.
I think we’re heading in that direction with informatics as well. The field is so vast that being a informatics generalist will soon be impossible because the information will be more than one person can reasonably be expected to handle. The influx of consumer technology and the need for better interoperability between systems will ultimately drive informatics pharmacists to specialize in one, or perhaps a few, specialized areas.
I consider myself an informatics generalist, but wonder how long before I won’t be able to keep up with new developments in the field. I’m already seeing signs of specialties within pharmacy automation and technology, it won’t be long now until we see it in other informatics areas.
Ultimately pharmacy informatics cannot be a specialty as the subject area by definition requires generalist knowledge. Eventually I think we’ll see practice specialties like we do in pharmacy practice today. Until then creating a pharmacy informatics specialty makes little sense.

 Several months ago I wrote about
Several months ago I wrote about 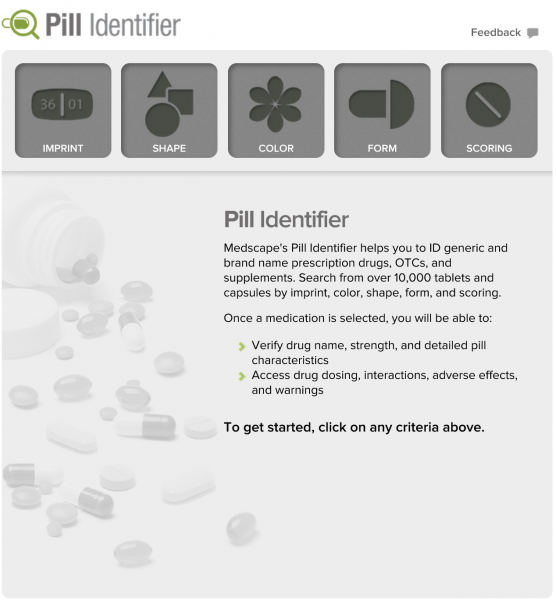 I received an email this morning from Medscape introducing me to their new
I received an email this morning from Medscape introducing me to their new