The DoseEdge Pharmacy Workflow Manager, formerly IntelliFlowRx Workload Management Software by Baxa, is a system designed to track and manage intravenous (IV) medication dosages prepared by pharmacy personnel in a clean room environment. The system is touted as “The world’s first and only fully integrated workflow manager for the IV room.â€
The system is designed to flow something like this:
– IV medication orders entered by the pharmacist, or other healthcare professional, are sent to the DoseEdge system where they appear on the DoseEdge touchscreen.
– When the technician, or pharmacist in some cases, accesses the order via the touchscreen instructions for preparation of the product are displayed.
– The product label is generated.
– The barcode on each injectable ingredient used for the preparation of the IV product is scanned to ensure the correct medications have been selected. Items identified as incorrect result in an audible message of “product not allowed for this dose.â€
– The barcode on the IV product label generated by the pharmacy is scanned to ensure that ingredients are appropriately matched.
– Each ingredient is drawn into a syringe.
– An image of the syringe with appropriately drawn medication is taken for review by the pharmacist, or technician, whichever the case may be. This is a nice feature as it allows one to see the actual amount of drug drawn into the syringe prior to shooting it into the fluid bag.
– Ingredients are injected into the fluid bag and an image of the final product is taken.
– A final scan of the product barcode is done to complete the fill.

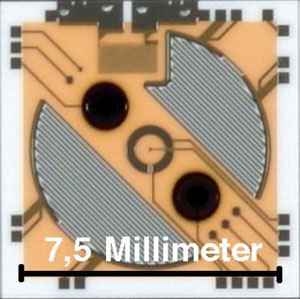
 CDEX’s technology stands alone, able to precisely identify medications in real time with its patented Enhanced Photoemission Spectroscopy technology.
CDEX’s technology stands alone, able to precisely identify medications in real time with its patented Enhanced Photoemission Spectroscopy technology. 2009 brought many new and exciting changes not only in my personal life, but in the world of pharmacy and technology as well. I’ve learned many new things, gained some skills previously absent from my armamentarium, met some great new people, discovered the “real†internet for the first time, traveled more than ever before, discovered I don’t know diddly squat about a great many things, and am more excited about the next year than I can remember in recent history.
2009 brought many new and exciting changes not only in my personal life, but in the world of pharmacy and technology as well. I’ve learned many new things, gained some skills previously absent from my armamentarium, met some great new people, discovered the “real†internet for the first time, traveled more than ever before, discovered I don’t know diddly squat about a great many things, and am more excited about the next year than I can remember in recent history.