 I’ve been following the Twitter stream from the ASHP Midyear in Tampa (#ashpsm10). Sunday morning I saw a Tweet from Karl Gumpper come through the ticker stating “ASHP Statement on Barcode on Inventory, Compound & Dispense approved by House of Delegates.†That’s a good thing.
I’ve been following the Twitter stream from the ASHP Midyear in Tampa (#ashpsm10). Sunday morning I saw a Tweet from Karl Gumpper come through the ticker stating “ASHP Statement on Barcode on Inventory, Compound & Dispense approved by House of Delegates.†That’s a good thing.
The ASHP Statement on Bar-code Verification During Inventory, Preparation, and Dispensing of Medications can be found here. I re-read the paper Monday morning. There is a lot of good information throughout the document, but I one paragraph in particular caught my attention. “In addition, for BCMA to function, a vast majority of doses must be accurately bar coded, meaning there must be a highly reliable relationship between the information in the bar code and the contents of the dose. Additionally, the bar code must be readable by commercially-available scanners. Although doses delivered directly from manufacturer-labeled packages generally meet these conditions, there are numerous drug products that may not.†This makes sense as a bar-code is useless if it can’t be easily read by a scanner. And believe me when I say that we find our fair share of bar-codes that don’t want to cooperate. The same can be said for bar-code scanners. I’ve heard people say that almost any of the new bar-code scanners today will do the job. I humbly disagree as I’ve had the misfortune of using some awful bar-code scanners on our way to settling on those currently used in our facility. Some of it is personal preference, but some of it is quality of the device. I’ve written about my opinion for consistency with scanning hardware before.
Just by chance, after reading the ASHP statement on bar-code verification, a nurse cornered me in the hall and informed me that the bar-code on one medication in particular was giving him a lot of trouble. It’s not uncommon for a nurse to curbside me regarding a bar-coding issue. I trust this nurse’s judgment and ended up in the pharmacy about an hour later looking at the offending agent. Sure enough, the drug in question was difficult to scan. It got me thinking about other medications that had bar-codes on their packaging, but for one reason or another were problematic.
So I started looking around the pharmacy and here are some of the things I found:
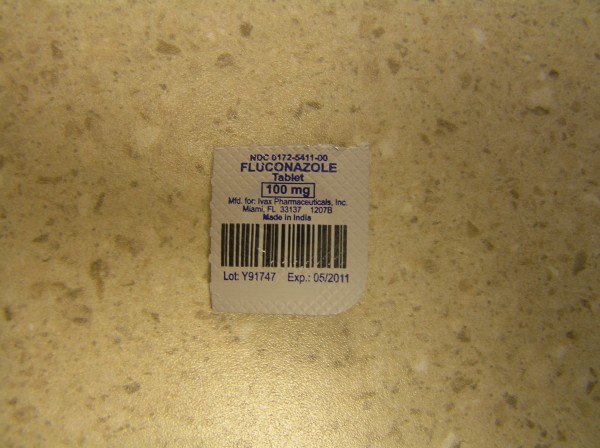
The packaging for the fluconazole tablet below is small and made of a material that reflects a lot of light. In addition to making the bar-code difficult to scan the packaging also makes the printing susceptible to scratches. Sometimes the scratches are bad enough to ruin the bar-code completely. Solution: change manufacturers if possible. If not consider purchasing in bulk and packaging ourselves; not the preferred thing to do as it adds an additional step to the dispensing process where error may be introduced.
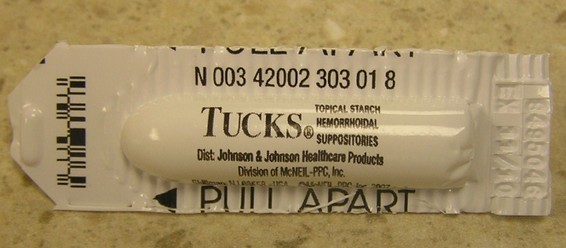
A lot of suppositories are manufactured with poorly designed bar-codes. The image below is shown exactly how it arrives from the wholesaler. The bar-code is very small and attached on the apex of a rounded surface, making it difficult to scan. Solution: change manufacturers. If that doesn’t work, we add our own circle label to the suppository; not the preferred thing to do as it adds an additional step to the dispensing process where error may be introduced.

The bar-code on this Tucks suppository runs along the left edge and it’s really small. Solution: see acetaminophen above.
Large volume parenteral solutions are difficult to scan because the scanners recognize the bag as a black background, thus the reason for the white bar-code. In addition the flexibility and location of the bar-code make it difficult to scan. Solution: still working on this one. For items compounded in the pharmacy we use the bar-code on the patient specific label for scanning. It’s the premixed solutions that give us trouble. Although I must say that the problem is less apparent now that everyone has had time to get used to the scanning process.

This jar of silver sulfadiazine cream is completely unscannable. It’s small and the color of the jar is problematic. Frankly, I couldn’t get it to scan a single time. Solution: change manufacturers, which we did. The bar-code on the new manufacturer is easily read by our scanners.

Labels near the edge of piggyback bags can be problematic because they wrinkle. This one isn’t too bad, but the bar-code needs to be relatively flat to get a good read. Solution: move the label up on the piggyback and get away from the edge. In the future I’d like to use a small 2D bar-code instead of the giant linear thing you see below. That functionality isn’t currently available in our pharmacy system.

We draw erythropoietin into syringes instead of sending vials; it’s a cost savings movie. In addition to a label identifying the drug, each syringe receives a second label identifying the patient specific dose. Both syringes below are poorly labeled. The one on the left because the bar-code is wrapped around the syringe, making it impossible to scan. The label on the right is better, but obscures the plunger in the syringe making it impossible to read the volume. Solution: education.

And finally the location of the bar-code on this pre-mixed bag of cefazolin causes problems because we teach the technicians to place the patient specific label just below the name of the drug, image on the right. Unfortunately, that results in the patient specific label covering the manufacturer’s bar-code. Solution: move the patient specific label to the back along with education.

Leave a Reply