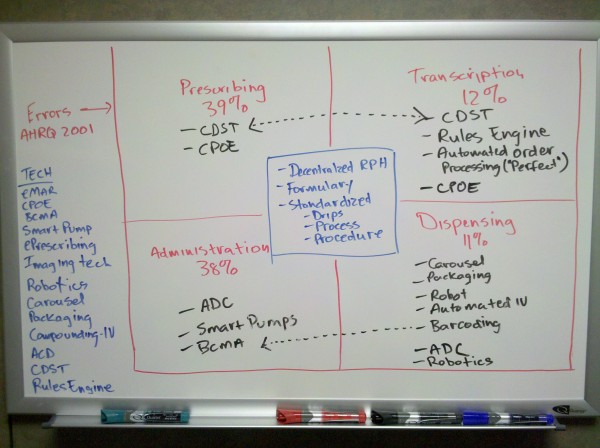
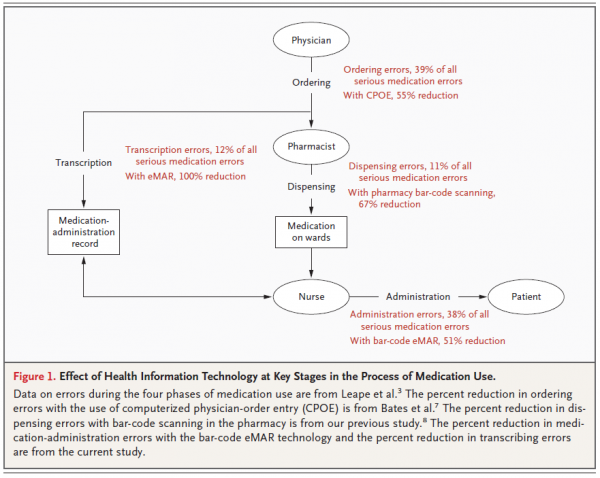
I’m not a big fan of the using the “best of†model for hospital information systems (HIS). You know, when you buy the best pharmacy system you can find, and the best lab system you can find, and the best ED system you can find, and so on. All this does is create a giant headache for everyone involved because the systems don’t always play nice with each other, which means data gets lost or hijacked between systems by the Interface Noid. Data gets pushed, moved, shuffled, altered, chopped and converted, and it doesn’t always come out the way you intended. Or worse yet, you have a case where the systems aren’t interfaced at all.
I’m not a big fan of the using the “best of†model for hospital information systems (HIS). You know, when you buy the best pharmacy system you can find, and the best lab system you can find, and the best ED system you can find, and so on. All this does is create a giant headache for everyone involved because the systems don’t always play nice with each other, which means data gets lost or hijacked between systems by the Interface Noid. Data gets pushed, moved, shuffled, altered, chopped and converted, and it doesn’t always come out the way you intended. Or worse yet, you have a case where the systems aren’t interfaced at all.
I recently heard of a case where a hospitals ED system wasn’t interfaced with the rest of the facilities information systems and disastrous results ensued. A patient came in through the ED with a very specific allergy; noted in the ED system. The information wasn’t available in the nursing or pharmacy systems. The patient was admitted and transferred to the floor. The little detail about the allergy wasn’t passed on during report and the patient ended up receiving that very medication based on the attending physician’s order. To make a long story short, the patient had an anaphylactic reaction and won a three day, all expenses paid trip to the hospitals intensive care unit.
I wonder how often things like this happen due to short sided HIS implementation and deployment. Technology might not be the answer to all our problems in healthcare, but you have to admit it certainly could have helped in this particular example.
 I’m not a big fan of the using the “best of†model for hospital information systems (HIS). You know, when you buy the best pharmacy system you can find, and the best lab system you can find, and the best ED system you can find, and so on. All this does is create a giant headache for everyone involved because the systems don’t always play nice with each other, which means data gets lost or hijacked between systems by the Interface
I’m not a big fan of the using the “best of†model for hospital information systems (HIS). You know, when you buy the best pharmacy system you can find, and the best lab system you can find, and the best ED system you can find, and so on. All this does is create a giant headache for everyone involved because the systems don’t always play nice with each other, which means data gets lost or hijacked between systems by the Interface