Two things happened to me recently that have pushed this question to the front of my mind.
The first is by way of some comments that were left in response to something I wrote in June about Google’s new symptom search. The comment is as follows:
“...I have to question your closing statement: The idea of such a vast amount of knowledge at one’s fingertips is mind boggling, to say the least. Google, like any reference, has “informationâ€, but I’m not sure if I would classify it as a “vast amount of knowledgeâ€. Actually, knowledge on the part of the reader is what is required to make sense of the information that a source like this provides. The ability to interpret drug literatures only comes with education, training, and experience…”
The second item comes from a Reddit thread that I got involved with a few days ago. In the thread a user asks whether or not a pharmacist could be replaced “by a computer†in another 20 years. I argued that it could certainly happen. Someone countered by saying that it couldn’t happen because “the evaluation side, the interpretation of a patient, taking it’s [sic] history into account†couldn’t be done by decision-making software.
Depending on which side of the fence you’re on, there is potential for some good discussion here.
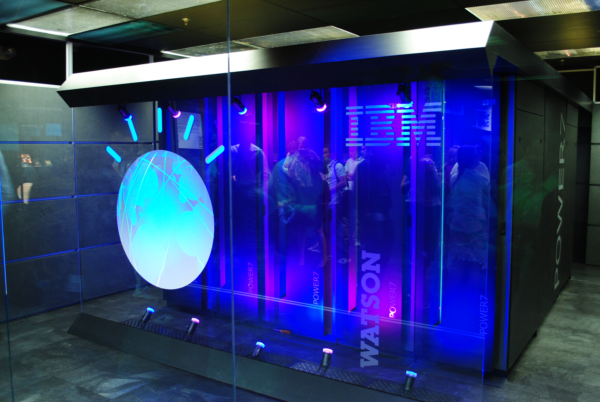
As I see it, information by itself holds little value. Having the skills to apply information to a given situation, i.e. “having knowledgeâ€* makes all the difference in the world. Many think that it is this that makes humans indispensable in certain roles, like pharmacists. However, don’t be too quick to dismiss the ability of artificial intelligence (AI) and machine learning (ML) to mimic the actions of a human, especially in healthcare. Both AI and ML are powerful tools that can be used to appropriately apply information to any given situation. If a piece of software is able to use ML and AI to apply information to a situation based on past experience, doesn’t this become “knowledgeâ€? I think it does.
This is what pharmacists do throughout their career – take what they’ve learned, add it to what they’ve experienced, and apply it to a given situation – and why seasoned veterans are so valuable. It’s not that they’re smarter than their younger counterparts; it’s that they’ve been around longer and seen more. The knowledge gained by veteran pharmacists is often the difference between making average decisions and making great decisions. As pharmacists practice, they gain more knowledge. As time goes by it becomes increasingly rare to see new situations. I’m sure that computers can take information and combine it with previous actions and outcomes to make decisions. They do it all the time.
Not all knowledge requires depth of logic and “freedom of thoughtâ€. Take for example a pharmacist that gains knowledge by reading through a new set of treatment guidelines, or a journal article, or by attending a conference lecture. After digesting the information – use drug x in this situation – the pharmacist is ready to apply it. This is one of the things that make pharmacists better as clinicians over time, i.e. learning new things from others. Can’t a computer use the same information and be given parameters from which to apply it? Sure. How is that different from a human pharmacist? On the surface it’s not.
So while I understand the desire for pharmacists to push back on the idea of being taken over by computers, I fundamentally disagree. I believe that 80% of what pharmacists do right now could be successfully emulated by a combination of technologies. Decisions made by pharmacists rarely require some special power of observation. Most are actually pretty cut and dry. What about those times that require a judgement call? That’s the other 20%. And while I think you need a pharmacist to make those calls today, I don’t think it will be long before technology can do the same thing. After all, most judgment calls are simply something learned plus experience. Computers may not be able to think on their own, but they can certainly take information, search for a previous encounter, and “make a decisionâ€.
Obviously this is just my opinion, take it for what it’s worth.
——————————-
*one definition of knowledge – “facts, information, and skills acquired by a person through experience or education; the theoretical or practical understanding of a subject.â€